Single embryo transfer (SET) is a proven option to achieve high pregnancy rates in young patients (Martikainen, H. et. Al., 2001). Introduction of PCR-based preimplantation genetic testing (PGT) can become a basis to expand SET to the older patient population. Precise evaluation of the genetic status of embryos should facilitate accurate embryo selection for the transfer (Handyside A., 2013).
The objective of this study was to compare pregnancy rates after SET for patients under 38 y. o. and over 38 y. o. in PGT cycles.
A retrospective study of SNP PGT pregnancy outcome data from single embryo transfers was conducted to identify differences in clinical pregnancy for patients ≤37 y. o. and ≥38 y. o..
195 cycles of IVF treatment with PGT between January 2013 and December 2014 were included in the study. In all cases only one euploid embryo was selected for transfer. All embryos were hatched on day 3 and were biopsied on day 5 or on day 6. Only good and fair quality embryos that had at least 3-7 herniating cells and met criteria for cryopreservation were considered for biopsy.
A total of 1072 embryos were analyzed for euploidy rates and blastocyst morphology. Morphology of blastocysts was evaluated by Gardner classification (Gardner et al., 1999).
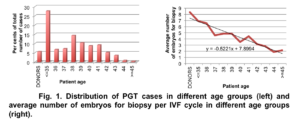
81 IVF cycles (69 patients) were included in the young (≤37 y. o.) patient group (average age – 33.25±3.29) and 114 IVF cycles (97 patients) in the older (≥38 y. o.) patient age group (average age – 40.68±1.67). The average number of embryos available for biopsy per case in the group of patient ≤37 y. o. was significantly higher than in the group of for patients ≥38 y. o.: 6.59±2.36 and 3.92±1.92 respectively, p<0.05. (Fig. 1).
Euploidy rate was statistically higher in young patient group than in older patient group: 56.32% and 37.55% respectively (p<0.05, χ2= 27.573) (Fig. 3).
We observed a strong correlation between euploidy rates and patient age. Euploidy rate decrease gradually with advancing maternal age (Fig. 3).
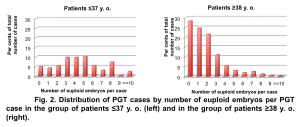
75 out of 81 SETs in the young patient group were elective SETs (two or more euploid embryos were available for transfer), while in the older patient group only 74 out of 114 SETs were elective SETs (Fig. 4).
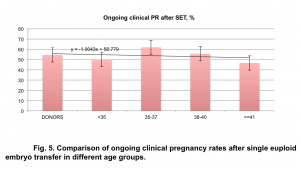
Analysis of ongoing clinical pregnancy rates in different age groups demonstrated no interrelation between maternal age and pregnancy rates after single euploid embryo transfer. Association between maternal age and pregnancy rates was assessed by identifying coefficients of linear regression: y = -1.0043x + 56.779 (Fig. 5).
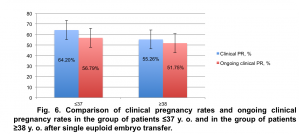
The ongoing clinical pregnancy rate for patients ≤37 y. o. was 56.8% (46/81). The ongoing clinical pregnancy rate for patients ≥38 y. o. was 51.8%, (59/114). The difference in pregnancy rate between two groups was not statistically significant: p=0.48698092, χ2=0.483191 (Fig. 6).
Our data demonstrated no statistically significant difference (p=0.5695, χ2=0.32275) in ongoing clinical pregnancy rates after SET between cases where only one euploid embryo was available for ET versus cases where two or more euploid embryos were available for ET in both study groups (Fig. 7).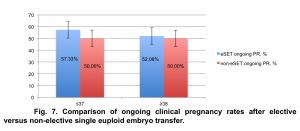
Conclusion
Analysis of the data proved effectiveness of preimplantation genetic testing for infertile patients of advanced maternal age. Single embryo transfer in PGT cases can significantly decrease multiple gestation rate without compromising clinical pregnancy rate regardless of patient age.
References